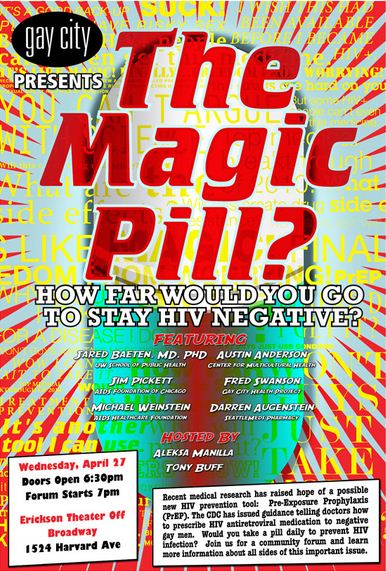
Reporter Christopher Jacquet investigates the “Great Hope” of the LGBTQ community and gets some answers on our most frequently answered questions from Seattle Public Health’s Dr. Joanne Stekler. AND, don’t forget “The Magic Pill” forum is TONIGHT at the Erickson Theater on Capitol Hill! And, it’s FREE!
Some of our community is known as “Men who have Sex with Men”, aka, “MSM”. It is a category used by the Centers for Disease and Control Prevention in order for epidemiologists to study the spread of disease and to identify an at risk group based on behavior. “MSM” allegedly make up two percent of the U.S. population, yet it holds statistics for, “Highest population most severely affected by HIV” and “Only risk group in which new HIV infections have steadily increased since the early 1990s,” according to the CDC website.
Strip down the category to a person, put a heart in place of the datum and you may see a face of someone who is HIV positive. Whether it is an acquaintance, a friend, a lover, or even yourself varies. But what is certain for our community is that recent research and discoveries have led to what many believe could be “The Magic Pill” to prevent the spread of HIV/AIDS. HIV medicines effective in treating HIV positive people, when used as a Pre-Exposure Prophylaxis, aka, “PrEP”, could have a preventive potential for HIV negative people when used before coming into contact with the virus. There is a chance that PrEP could save the lives of thousands, if not millions of people around the world.
Gay City Health Project is hosting a free forum for the public about PrEP to discuss the hopes and fears for “The Magic Pill” (Truvada) that could greatly reduce the percentages of infection in our community. The forum will be held Wednesday, April 27 at 7pm (doors open at 6:30pm) at Erickson Theater off Broadway, 1524 Harvard Ave, behind the Egyptian theater. Hosting the forum will be Seattle performer, Aleksa Manila and erotic film star, Tony Buff, both active members in the local and national fight against HIV/AIDS.
Whether you’re a leatherman or a drag queen, HIV does not discriminate. (It’s important to have) a Desire to know (the facts) so that we, as a community, can make healthy choices… Aleksa Manila
The experts and local leaders in HIV/AIDS prevention that will be speaking at the forum, include:
Jared Baeten, MD from UW School of Public Health
Jim Pickett from AIDS Foundation of Chicago
Michael Weinstein from AIDS Healthcare Foundation
Austin Anderson from the Center for Multicultural Health
Darren Augenstein from SeattleMeds Pharmacy
Presiding over the seminar will be Gay City Health Project Executive Director, Fred Swanson, who stresses the importance of this information when responding to questions gathered from a concerned and interested community: “The point is that different people respond to different alternatives…No solution is foolproof or without problems; having more options available is a good thing.”
So what is PrEP and how is it different from other alternatives?
Dr. Joanne Stekler, an HIV Doctor at Public Health in Seattle gives insight to questions for a HIV negative, gay male who is concerned about the CDC issuing help to doctors prescribing Truvada as a form of HIV prevention.
Dr. Stekler answers our questions, after the Jump…
Q: What do I need to know about PrEP?
Points from Dr. Stekler:
- PrEP works if taken it before coming into contact with HIV.
- The iPrEx study was the first PrEP study to release results in November 2010. The iPrex study showed a 44% reduction in new infections.
- The pill used during iPrEx is Truvada, which is antiretroviral drug, a combination of tenofovir and emtricitabine (two medications used to treat HIV infection). By combing the two agents into a tablet it reduces the pill burden and increases compliance for patients. However in some studies that are using just tenofovir.
- Adherence to medications shows a 73% effect for subjects who took the pill at least 90% of the days.
- 3% of subjects still got infected with HIV despite receiving PrEP.
- PrEP is not a substitute for condoms, having few or one partner, getting regularly tested and talking to partners about HIV/STD status.
“I think this was a really exciting study,” Stekler said. “But it’s only the first of its kind, and so we’ll have the results of several other PrEP studies in a variety of populations (i.e. heteros, injection drug users) in the next few years.”
Q: What are the damages? The risks?
Dr. Stekler: “The main side effect of PrEP is pain in the pocket book.”
- There is still uncertainty about insurance coverage.
- The anticipated cost for the medicines alone, out of pocket is over $10,000.
- The main physical side effects include: nausea, weight loss, and slight kidney problems.
- There is concern with drug resistance: “The ability for HIV to mutate and reproduce itself against antiretroviral drugs,” defined by the World Health Organization.
- If someone gets infected while taking PrEP, they are only using two pills instead of the three that are used for someone with HIV. This is a way HIV resistance can be developed.
“In an era of greater and greater budget cuts, with more states having waiting lists or restricting eligibility for ADAP, Public Health does not anticipate funding a PrEP program, but there are a lot of equity and social justice issues that are highly relevant to the topic that we want to pay attention to,” advised Dr. Stekler.
Another option for HIV prevention is PEP (Post-Exposure Prophylaxis). If PrEP can be seen like a daily “Birth Control Pill” to reduce risk, then PEP could be compared to the “Morning After Pill” for HIV exposure. PEP is not a daily pill, but taken when needed for a set number of days for incidences such as: broken condoms, drunken “mistakes”, and victims of rape and sexual violence.
Q: Tell me about PEP. How does it differ from PrEP and who is it for?
Dr. Stekler: “Folks who are repeatedly exposed to HIV, taking PrEP every day is like taking PEP over and over again. The main difference is that PrEP is only one or two HIV meds and PEP is usually given as a three drug cocktail. Whether that makes a difference for efficacy, we don’t know.”
- PEP (Post-Exposure Prophylaxis); for people who may have come into contact with HIV.
- It was first given for occupational exposures to HIV for medical personnel in the case of needle pokes.
- PEP will usually not be given after 72 hours of possible infection.
- It is really important to start a HIV regimen for up to 28 days as close to the time of exposure as possible (the closer to the 48 hours, better).
- The success rate is as high as 80%.
“It’s available,” Dr. Stekler continues; “through private providers, or at the Madison Clinic at Harborview.” More information can be found PEPnow.org and PEP411.com.
There is another option on the verge of a study, so keep your eyes open for its progress and release. It is known as MTN, aka, Microbicide Trial Network. “There has been a lot of interest in developing a microbicide that could be used as a topical gel, vaginally or rectally, in order to prevent HIV infection,” Dr. Stekler notes.
Q: What do we know about “MTN”? Will it be in lube form?
Points from Dr. Stekler:
- There have been a lot of negative studies (nonoxy19) when developing a microbicide.
- Finally in 2010, CAPRISA study presented the first results of an effective microbicide against HIV infection in heterosexual woman.
- The microbicide is used with intercourse as a lube mixed with tenofovir, which gave 39% decrease in risk of infection.
- Important note: A study is being reformulated for a rectal gel. A side effect in the rectal cells that is being resolved is osmolality, which is a process that causes the cells to expel water and become damaged.
- According to the AIDSmeds.com website, by reducing the amount of silicon in the gel the osmolality can be reduced. That discovery has led to a new study.
- Just announced on April 18,2011: The FEM-PREP study – which was a study of PrEP in women – was stopped early because of futility (Futility means that the study as designed was never going to be able to show a difference between PrEP and placebo).
Stekler adds, “ I don’t know much about the reworked rectal formulation. The microbicide folks want any gel they develop to be not unpleasant tasting and to function as lube.” The microbicide is currently unavailable, but knowing that it could be a future option is what matters.
Gay City’s Fred Swanson says, “A good solution for one person doesn’t mean we stop exploring alternatives for others.” So the question really is, “What is right for you?” To give you the best answer, come attend the Gay City forum “The Magic Pill” next Wednesday, April 27. For more information on the event, visit the Gay City website.